In the United Kingdom's National Health Service, 50 percent of health care workers do not get flu vaccines. Obviously they are not anti-vaccine, they work in health care, so what explains their behavior? It isn't as simple as science denial.
In the United States, vaccine denial is easier to predict: Go to a political map of California or Oregon and find the counties that voted overwhelmingly for President Obama and you are going to find an anti-vaccine hotbed. Still, though that tells us where it does not tell us why and we need to know why in order to know how to solve the problem. It isn't as simplistic as 'Democrats are anti-science', though it is reasonable that it's been framed that way.
We know the hotbeds are in states that vote Democratic but that doesn't make Democrats anti-science. Maryland is the most politically lopsided state in the continental US for Democrats but their exemption rate is only 1%. Democrats insist they accept science but attempts to imply that Republicans are also anti-vaccine and anti-GMO have been non-starters. The numbers don't add up.
Yet there are some areas where Republicans are as anti-science as Democrats and that may show us how to get better uptake and protect people who can't get vaccines for medical reasons.
Are you an anti-vaxxer if you don't get the flu vaccine?
I've never had a flu vaccine. I am obviously not anti-vaccine, and when I am older, I certainly will, because my risk of harm is higher. For now, I work in my house so I am unlikely to get the flu and I am even less likely to be exposed to someone who has an immune issue. Being paralyzed by the precautionary principle given those parameters gets to be tinfoil-hat stuff, when only 5 percent of the public is going to get the flu. Year-round, 'I have the flu' is an even more exaggerated medical claim than 'I have gluten intolerance'. If you are sick for a few days, you have a respiratory syncytial virus, a coronavirus or an enterovirus, but the flu is serious stuff and the annual vaccine is designed to prevent the A and B versions.
Some years, the flu vaccine does not work very well, and yet people are told to take it anyway. That does not increase the public's confidence. Flu vaccines can tell us why some people go overboard and deny all vaccines, especially if we try to find out:
Are you an anti-vaxxer if you didn't get the HPV vaccine?
HPV, the , is designed to prevent a rare cancer from a common virus, along with genital warts. Yet in the United States only 35% of young girls have gotten the vaccine, even though 84 percent of girls who have not been vaccinated for it visited a doctor for a different vaccine. That means the parents are not anti-vaccine, and the lack uptake is so high we can't really pin down what kind of person does not opt for it. Cervical cancer is rare and about 4,000 women die from it each year and 3,500 people die each year from accidental drowning, to put that number in perspective.
In the cases of the flu and HPV and we can add in Shingles or anything else, if we shriek anti-vaxxer at someone who does not get them, we engaging in the silly sort of false equivalence that makes the public distrust science media. All denials are not equal because all problems are not equal. Jonas Salk got 1,800,000 school children in the clinical trial for his polio vaccine - that was before it was even approved. The results were announced in 1955 and by 1957 everyone was using it.
Polio was serious stuff.
Are you an anti-vaxxer if you didn't get the polio vaccine?
Polio is what put routine vaccination on the map and it's nice to think polio is basically extinct, thanks to vaccines, but that isn't really so. In 2013, an outbreak occurred in Israel and and to prevent paralytic polio the Israeli Health Ministry launched a campaign to immunize children under the age of 10 with a bivalent oral polio vaccine and insure "herd immunity" for those not already vaccinated.
Some parents who were not previously vaccine refusers and who had complied with routine vaccination programs refused to vaccinate their children.
How can they be anti-vaccine if they are clearly pro-vaccine?
There are two cultural forces at work, one is among groups and one is among individuals. But until we find a way to solve those we may never have the kind of acceptance we want.
The group problem: People are being taught to distrust doctors and pharmaceutical companies
Hardly a week goes by that doctors or drug companies are not criticized. John Oliver on “Last Week Tonight” uses some statistic to create causation and implies that doctors are so unethical, they can be bribed with a lunch, or even a compliment - because they often prescribed new drugs after meeting with a pharmaceutical rep whose job it is to explain the benefit of a new drug.
And this chart criticizes drug prices
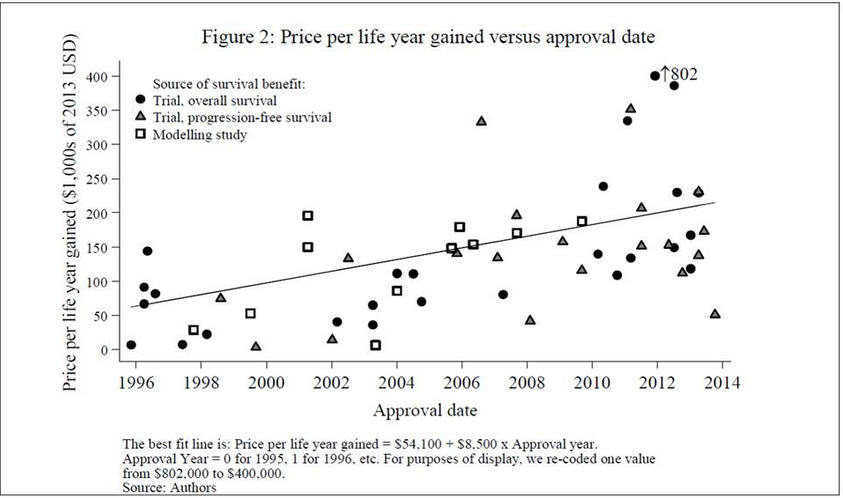
Link: Mark Schoenebaum
So tell those anti-vaccine people again why they are supposed to trust doctors and scientists and drug companies when doctors and scientists and journalists gleefully post this stuff on social media.
America is, at heart, a nation of skeptics, as infuriating as that may be when people disagree with what we know to be true. So if you are in science media or science or medicine and you just got done criticizing Merck for its marketing budget, how can you then turn around and tell people they are anti-science if they don't get an HPV vaccine - created by Merck and marketed heavily right after they lost $5 billion on a Vioxx settlement for something that only kills slightly more people than swimming pools do?
I have no issue with Merck selling one new product when they pay off lawsuits for an old one, but I know how hard drug discovery is and I also know how easy it is to file a lawsuit and get a lot of money. They are completely separate groups and Merck, like most companies, will have 19 expensive failures for each success - and even then they can't anticipate everything. But the public is not going to do that level of research, all they see is the vilification of mainstream medicine and the pharmaceutical companies that make it happen.
It isn't homeopaths or nutritionists creating doubt about medicine, it is us.
The individual problem: People want to emulate those they admire
We all know that 'thought leaders' exist, it is why people pay for celebrity endorsements. It is unlikely that conservatives drank much tea in the United States - we went to war with the British over that vile leaf over 200 years ago - yet when he endorsed a brand of tea, sales of the product skyrocketed. People in his audience are inclined to listen to his recommendations because he is a smart guy and they admire him.
California progressives who are against vaccines also have role models they aspire to being, but rather than flocking to smart white men, they flock to pretty white women. You think Uggs were some great brand of shoe? No, they got celebrities to wear them and they took off from there. No designed is selling any men's clothes due to the Academy Awards red carpet later this month, but every woman wants to know
You can bet wealthy progressives were going to be first in line to get an Ebola vaccine if deaths had begun to climb here, no mumbo-jumbo about breastfeeding and organic food making vaccines irrelevant
. People trusted science and the big reason was that there was no political infighting between government-funded academics and private sector researchers. How often do we see allegations that a study is not legitimate if it was funded by a company?
Yet they have gotten most of the other vaccines for their kids and strongly believe in them.
California leads the country is vaccine denial and voted for President Obama but so did Maryland, and their vaccine exemption rate is only 1 percent. Not as good as Republican states like Mississippi and Alabama but not a crisis either.
What makes California different from Maryland is celebrity worship.
To get vaccines back on track, it may be wise to do what made Uggs popular: Get cool people to do it.
Some of the arguments that vaccine denial is bipartisan use broad geographies to dilute defined pockets. Modern revisionism of California's 2008 measles outbreak, for example, makes the claim that because it was San Diego county it must be Republicans being anti-vaccine.
If we are being honest, a lot of the anti-vaccine sentiment is due to the fact that the political demographic most likely to be anti-vaccine are also most likely to want to emulate celebrities. A lot of wealthy elites in California want to do what Hollywood actresses do; if a section of Los Angeles that has a lot of Hollywood celebrities just happens to be a hotbed of autism (it is - kids move there and suddenly get diagnosed) you can see that pockets of Marin and San Francisco and Berkeley did the same thing after it became a popular trend. Now that Jenny McCarthy has moved on from autism, we can get someone pretty and famous to fill that void.
I am not saying we shouldn't shame people into doing the right thing - despite cries that sentence is going to get, shame is a time-honored way to get people to stop being selfish or stupid. But shame will only get you so far, and so will earnest public service announcements.
Does Amanda Peet have the Hollywood credibility to make vaccines popular among progressive elites again?
What instead will work best is targeting the cool kids in culture? In the case of California progressives, that means celebrities. A study in The Lancet used data from social connections of medical school students and then simulating vaccine approaches. Time and again the model showed that uptake was stronger if the popular people were vaccinated instead of random people.
http://www.bloomberg.com/news/2010-07-27/merck-paid-3-468-death-claims-t...
Anti-vaccine sentiments are overwhelmingly ideological. You can put a map over a political demographic and have a good idea whether or not it will be a vaccine hotbed, just as you can do about climate change.
Unlike climate change, where people are proud to embrace skepticism and critical thinking in their ranks, political writers who promote the notion that science votes Democrat scramble to rationalize that anti-vaccine beliefs are bipartisan. This requires some real intellectual gymnastics, like believing that all those counties full of wealthy white liberals refusing vaccines are somehow offset in Republican states. Texas, for example, has quite a few kids unvaccinated.
The CDC tracks vaccination coverage for many vaccines but it is not telling the correct story to infer that a poor person in Texas who does not have all of the vaccines for a child at 19 months of age is the same as a wealthy elite in California who sends children to public school without them. Anti-vaccine sentiment is when they intentionally exempt their children.
Anti-vaccine sentiment is beginning to fade. It is hard for progressives to claim they care more about poor people and then say they are not going to give their own children vaccines because poor children are the experimental lab rats. California is tired of having the country think that places like Los Angeles and the San Francisco-Berkeley woo nexus represent all 30 million people. And when the ebola hype was taking the country by storm, you can be sure the wealthiest California elites were going to make sure they were first in line for a vaccine.
But forgetting the misguided ideas about medicine and immunology that afflict the bulk of the anti-vaccine movement, there are some people who believe in vaccines, they just are not going to rush to get every new one.
That doesn't make them a dangerous anti-vaxxer. It makes them skeptical. Why would someone who has dutifully given their child every vaccine balk at a new one? It may be that Company Y just got sued for Product X and lost a big judgment and then rolls out Vaccine D in an expensive marketing campaign, that doesn't inspire confidence. Vaccines have a different level of proof for harm than regular drugs so if Merck loses a $5 billion judgment and suddenly rolls out a new vaccine,
Their confidence may also be shaken by how we talk about pharmaceutical companies. It is very difficult to imply that only government-funded scientists are ethical and then expect the public to embrace private sector products.
And the private sector is the only group that can produce drugs. If government controls drug research, a new version of aspirin will take 35 years and cost $50 billion.
As Samuel Broder, former Director of the National Cancer Institute, phrased the difference between government-controlled science and the private sector kind, "If it was up to the NIH to cure polio through a centrally directed program instead of independent investigator driven discovery, you'd have the best iron lung in the world, but not a polio vaccine."
A new study by Dr. Anat Gesser-Edelsburg, Dr. Yaffa Shir-Raz and Prof. Manfred S. Green from University of Haifa, School of Public Health, published in the Journal of Risk Research suggests that even parents who are not "vaccine refusers" and who usually comply with the routine vaccination programs may hesitate or refuse to vaccinate their children based on poor communication from the relevant healthcare provider, as well as concerns about the safety of the vaccine.
The issue of vaccination hesitancy and refusal often makes headlines in the media and worries
health authorities. However, a new study by Dr. Anat Gesser-Edelsburg, Dr. Yaffa Shir-Raz and Prof. Manfred S. Green from University of Haifa, School of Public Health, published in the Journal of Risk Research suggests that even parents who are not "vaccine refusers" and who usually comply with the routine vaccination programs may hesitate or refuse to vaccinate their children based on poor communication from the relevant healthcare provider, as well as concerns about the safety of the vaccine.
The study examines parents’ refusal or hesitancy to vaccinate their children following the 2013 polio outbreak in Israel. While no clinical cases of paralytic polio were recorded during the outbreak, the Israeli Health Ministry launched a campaign to immunize children under the age of 10, who were already protected with the standard inactivated polio vaccine (IPV), with a bivalent oral polio vaccine (OPV) designed to protect others who were not already vaccinated against the disease.
The study draws on results from a questionnaire survey, and content analysis of parents’ discussions in blogs, Internet sites, and Facebook.
Although the rate of children vaccinated during the campaign was high, the study's findings indicate that for the first time, parents who are not "vaccine refusers" and who usually comply with the routine vaccination programs, hesitated or even refused to vaccinate their children. One third of parents surveyed, who refused or were hesitant to vaccinate their children, reported that the safety of the vaccine was a concern, and that they were not convinced by the information communicated by the Health Ministry, or the explanation of why this vaccine was necessary.
Over a third of all respondents strongly disagreed that the Health Ministry had provided comprehensive and clear information about the reasons for giving children the vaccine, and almost 28% of parents who vaccinated their children indicated that they did not actually understand that the purpose of the vaccine was not to protect their own child.
The researchers went on to suggest that, in the long term, the perceived ambiguity in communications could create mistrust in the health care system. The theme of distrust in the medical establishment recurred in the analysis of 35 respondents who had refused or were hesitant about vaccinating their child.
This case emphasizes the importance of transparency and credibility in health communication. For example, The Health Ministry claimed that the OPV vaccine had ‘zero side effects’. Findings indicated that claiming there is no risk whatsoever was interpreted as neither respecting the public or credible. The researchers recommend that in future instances the risk-communicating organizations should ‘expose the dilemmas, communicate facts, and ‘talk science’ even to laypeople, especially in conditions of uncertainty: the communicators must educate the public and include it, and not speak in all-or-nothing slogans’.
http://www.tandfonline.com/doi/full/10.1080/13669877.2014.983947
Full bibliographic information
'Why do parents who usually vaccinate their children hesitate or refuse? General good vs. individual risk', Anat Gesser-Edelsburg, Yaffa Shir-Raz&Manfred S. Green, Journal of Risk Research, 10.1080/13669877.2014.983947.


