Co-authored by by Lauren Philippi, Department of Human Health and Nutritional Sciences, University of Guelph
In late December 2019 an outbreak of
pneumonia cases arose in Wuhan, China. Patients presented with an acute
respiratory illness linked to the 2019 Novel Coronavirus (COVID-19). COVID-19
is a betacoronavirus, similar to Human Severe Acute Respiratory Syndrome (SARS)
and Middle Eastern Respiratory Syndrome (MERS) coronaviruses. SARS and MERS
both cause severe respiratory disease. Although COVID-19 is primarily
considered a respiratory virus, there is a strong link to cardiovascular
disease.
COVID-19 — by the numbers
As of March 27, 2020, there are 509,164
confirmed cases and 23,335 deaths globally, with numbers changing rapidly (1).
The mortality rate and illness severity of COVID-19 remains low compared to
MERS and SARS. However, patients with pre-existing cardiovascular disease are
linked to 2 in 5 hospitalizations for COVID-19 (2). Mortality rates for
patients with cardiovascular disease exceed 10%, which is 50% higher than those
with respiratory conditions, and almost 5X the overall mortality rate.
The Beginning and The End
The immune system plays a vital role in
cardiovascular disease, including atherosclerosis, heart attacks, and heart
failure. Infectious diseases use the compromised immune systems of
cardiovascular disease patients to opportunistically invade the body. Conversely,
infections may activate the immune system and cause damage to the heart or
vasculature.
Early studies reported cardiac damage
associated with COVID-19 infection. Data from 1,527 patients across 6 studies
found that up to 11.4% of patients who tested positive for COVID-19 exhibited
signs of cardiac damage (3). In more severe cases from the ICU the rate of
cardiovascular disease was 13X higher. Shi and colleagues examined the medical
records of 416 patients hospitalized with COVID-19 in Wuhan and found 19.7% had
laboratory findings consistent with cardiac injury (4). The mortality rate in
patients with cardiac injury was 51.2%, versus 4.5% for those without.
The Key…
Could the cardiovascular system be the key
to solving the COVID-19 problem?
Studies of the related SARS coronavirus
showed that cellular entry is mediated through ACE2 proteins (5). ACE2 is a
homologue of ACE, which is most widely known for its role in regulating blood
pressure and as a causative player in hypertension. The role of ACE2, however,
is less clear (6). SARS uses a spike protein to bind to ACE2 and initiate
infection of cells (7). SARS-CoV-2, the virus responsible for the COVID-19 pandemic,
has a similar spike protein which suggests that the two betacoronaviruses share
a similar mechanism of infection.
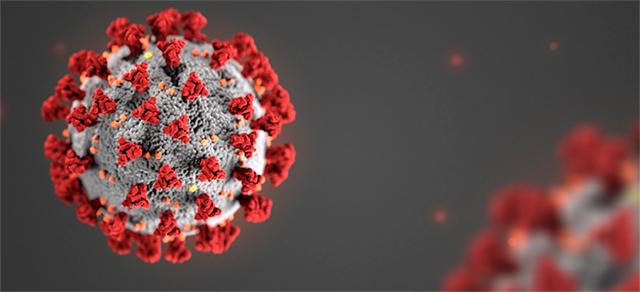
Image: CDC
Some have speculated that ACE inhibitors, a
class of drugs used to treat high blood pressure, may increase the risk of coronavirus
infection. Rodent studies showed that ACE inhibitors increase the expression of
ACE2, which in theory could provide additional entry points for viral infection
(8). However, this effect was not seen in human studies (9, 10). A number of
cardiovascular societies including the European and Canadian Societies for
Cardiology, along with the Hypertension Canada have strongly cautioned against
stopping ACE inhibitors without conclusive evidence for any impact (11-13).
In a letter published by the Journal of
Hypertension, Drs. Murray and Danielle Esler cite studies showing that
angiotensin receptor blockers (ARB) substantially increase ACE2 expression in
the kidneys and heart (6). ARB are another group of drugs that are commonly
used to treat hypertension. Increased infection in the heart could explain some
of the reports of cardiac damage associated with COVID-19. But, again, it
should be stressed that these studies were done in rodent models and there is
no clinical evidence to warrant changes in the use of ARB.
…Or the Obstacle?
The World Health Organization announced the
global SOLIDARITY trial to test four potential COVID-19 therapies: chloroquine
or hydroxychloroquine; remdesivir; lopinavir and ritonavir; and a combination
of lopinavir-ritonavir and interferon-beta (14).
SOLIDARITY builds off earlier studies that
identified these candidate treatments. A small open-label non-randomized
clinical trial reported some benefits of hydroxychloroquine-azithromysin treatment,
but the study was underpowered, excluded 4 patients in the treatment group who
died or were transferred to ICU, and has been plagued with allegations of
scientific misconduct (15). An earlier letter to Bioscience Trends reported
similar success, but detailed results were not published (16). Remdesivir showed
some effectiveness in two, single patient reports (17, 18), whereas a report
published in the New England Journal of Medicine found no benefits of lopinavir-ritonavir
treatment, potentially because the advanced state of illness may have been too
much for the therapy to overcome (19).
While SOLIDARITY offers hope for the
discovery of an effective therapy, concerns about the cardiovascular side-effects
of some treatments present significant and real obstacles. Hydroxychloroquine
increases the risk of ventricular arrhythmias and sudden cardiac death. Short
duration (5 days) lopinavir-ritonavir treatment decreases insulin sensitivity
which could impact cardiac metabolism (20). Prolonged lopinavir-ritonavir treatment
causes dyslipidemia and increases the risks of coronary artery disease (21),
and heart attacks (22). These dangers may not be an issue with the shorter
treatment duration expected in the SOLIDARITY trial. But the risks of
arrhythmias and cardiac stress should be carefully considered for all treatment
options, given the high rate of COVID-19 patients with pre-existing
cardiovascular conditions.
The Path Forward
COVID-19 presents a real risk to global
health, in large part through its potential to overwhelm the healthcare system.
It is clear that the primary target of the novel coronavirus is the respiratory
system. But the role of the cardiovascular system as a player in the
pathogenesis of the virus, a risk factor in morbidity and mortality, and as an
obstacle for treatment positions it as a critical factor in the management of
this global pandemic.
References:
1. WHO Situation Report, March 27, 2020.
https://www.who.int/docs/default-source/coronaviruse/situation-reports/…
2. Chen N et al. Lancet. 395: 507-513.
2020.
3. Li B et al. Clin Res Cardiol. In press,
2020.
4. Shi S et al. JAMA Cardiol. Published
online March 25, 2020.
5. Du L et al. Nat Rev Microbiol. 7:
226-236. 2008.
6. Esler M and Esler D. J Hyperten. March
11, 2020. In press.
7. Menachery VD et al. Nat Med. 21:
1508-1515. 2015.
8. Ferrario
CM et al. Circ. 111: 2605-2610. 2005.
9. Ramchand J et al. PLoS ONE. 13:
e0198144. 2018.
10. Walters TE et al. Europace. 19:
1280-1287. 2017.
11. CCS. COVID-19 and use of ACEi/ARB/ARNi
medications for heart failure of hypertension. March 16, 2020.
12. ECS. Position Statement of the ESC
Council on Hypertension on ACSE-Inhibitors and Angiotensin Receptor Blockers.
March 13, 2020.
13. Hypertension Canada. Hypertension
Canada’s Statement on: Hypertension, ACE-Inhibitors and Angiotensin Receptor
Blockers and COVID-19. March 13, 2020.
14. Kupferschmidt K and Cohen J. Science.
WHO launches global megatrial of the four most promising coronavirus
treatments. March 22, 2020. doi:10.1126/science.abb8497.
14. Kupferschmidt K and Cohen J. Science.
WHO launches global megatrial of the four most promising coronavirus
treatments. March 22, 2020. doi:10.1126/science.abb8497.
15. Gautret P et
al. Int J Antimicrob Agents. March 20, 2020. In press.
16. Gao J et al. Biosci Trends 14: 72-73. 2020.
17. Holshue
ML et al. N Engl J Med. 382: 929-936. 2020.
18. Cohen J. Science. Did an experimental
drug help a U.S. coronavirus patient? March 13, 2020.
doi:10.1126/science.abb7243.
19. Cao B. N Engl J Med. March 18, 2020. In
press.
20. Noor MA et al. AIDS.18: 2137-2144. 2004.
21. Limsreng S et al. PLoS One. 11:
e016306. 2016.
22. DAD Study Group. N Engl J Med. 356:
1723-1735. 2007.