After 20 years of grueling research, unimaginably effective drugs to treat hepatitis C are hitting the market. They are so good that cure rates (aka sustained virological response, or SVR)—defined as the absence of detectable hepatitis C virus (HCV) RNA six months following cessation of treatment—are approaching 100 percent. Even ten years ago this would have been regarded as science fiction.
These drugs are quite expensive. But, are they worth it?
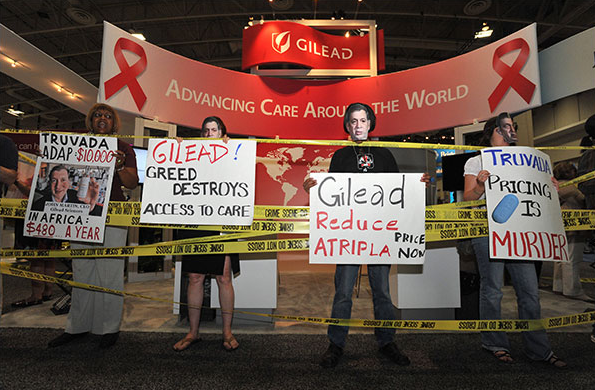
The fallout from the pricing of these drugs was inevitable, and closely mirrors what happened with HIV/AIDS about 15 years ago. Following a massive ten year campaign, which included contributions from virtually every major pharmaceutical company, drugs that could stop or slow the replication of HIV (and extend the life of HIV-positive patients) became available. These drugs were also expensive, and AIDS activist group showed their displeasure by, among other things, chaining themselves to the fences surrounding the homes of the CEOs of some of the companies that were selling the drugs.
I am not aware of any fence chaining, but criticism of the price of HCV drugs—especially Gliead's Sovaldi, which costs $1,000 per pill—is fierce. In fact, the May 7th Medscape daily email entitled "Hepatitis C: Cure, but at what cost?" featured nine articles about the high cost, including "Costs to Public of USD 84,000 Hep C Drug 'Outrageous,' and "WHO Joins Clamor to Make New Hepatitis C Pills Affordable."
So, are these new drugs too expensive? I guess that depends on whether you're buying or selling them. But, in order to determine the actual value of something like Sovaldi, you have to look at what it replaced—a therapy that was very difficult to tolerate, only modestly effective, and also rather expensive.
The
standard of care for hepatitis C only two years ago was a combination of
interferon and ribavirin, and it was god awful—mostly due to the interferon. In
his blog, "Antibiotics-the
Perfect Storm," Dr. David Shlaes, the former head of
infectious disease research at Wyeth elaborates: "Before Gilead’s Sovadi,
the standard treatment was 24 – 52 weeks of interferon plus
ribavirin. Interferon causes fever, chills, depression, low blood
counts and a number of other problems. It has to be administered by
intravenous injection monthly. Other drugs have to be used to counteract its
side effects. Ribavirin is given as a pill (many pills) and causes anemia among
other things. Sometimes transfusions are required to maintain blood
counts throughout a course of therapy. And after you have finished the entire
course, the failure rate of this therapy can be as high as 50%."
And let's not forget the
costs of not using Sovaldi. A course of Interferon plus
ribavirin costs $30,000. A liver transplant will set you back more than $500,000.
And the anti-rejection drugs needed after the transplant cost $20,000 for the first year
following transplantation.
All of a sudden the 84K doesn't seem so bad, does it? And Sovaldi is the only
interferon-free therapy that is approved by the FDA for treatment of
hepatitis C. The first generation HCV protease inhibitors, Incivek (Vertex) and
Virtrelis (Schering/Merck) significantly improved the cure rate, but these were
only approved for use in combination with interferon—not in place of it.
Other companies, notably AbbieVie, whose ABT-450 is expected to gain FDA
approval soon, are studying interferon-free HCV drug combinations. These drugs
will also be expensive.
But as Dr. David Berstein, chief of hepatology at the Center for Liver
Disease, North Shore University Hospital, Manhasset, New York, and co-author of
a paper in the May 4th New England Journal of Medicine said in a recent interview, “We in this country look at cost,
because it costs a lot. But you are curing 97% percent of patients in 12
weeks–so, what is the value of that?”
This is no time to fool around. These drugs have the potential to wipe out hepatitis C, which has infected three million Americans, and 170
million people worldwide—about four times that of HIV.
No- new hepatitis C drugs are not too expensive. They are
appropriately expensive. Advances like this come up once in a lifetime. The
companies that devoted many years and spent billions of dollars to make this
happen should be rewarded. And when you factor in the high cost and high
failure rate of the previous treatment, this actually becomes a bargain.